What is Systemic Inflammation?
Systemic inflammation is a chronic immune response that affects the entire body rather than just one area, like a localized injury or infection.
Unlike short-term inflammation, which helps healing, this kind of inflammation persists over time, often without obvious symptoms at first. This ongoing immune activation can cause widespread irritation in tissues and organs and may eventually impact quality of life.
From a biological perspective, it is marked by:
- Erythrocyte sedimentation rate (ESR) and sometimes elevated inflammatory markers in the blood, such as C-reactive protein (CRP)
- Increased activity of immune cells, including signaling molecules called cytokines and sometimes white blood cells
- Sometimes, higher levels of eosinophils, a specific type of white blood cell
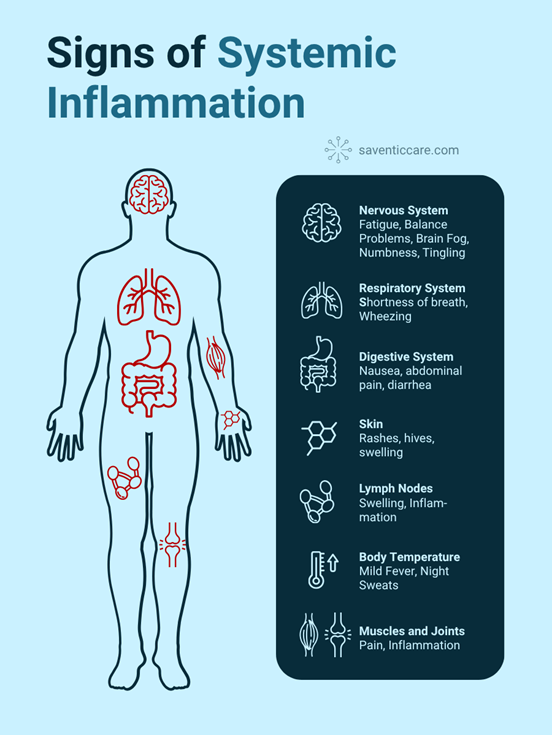
Warning signs
When the systemic inflammation is chronic, signs can be subtle and easily mistaken for stress, aging, or other conditions. But, over time, they may worsen. Common signs include:
- Muscle and joint pain
- Swollen Lymph Nodes
- Shortness of breath or wheezing
- Skin rashes or sensitivity
- Digestive disturbances
- Mild fever
- Night sweats
- Long-lasting fatigue
- Balance Problems
- Brain fog or difficulty concentrating
- Numbness, tingling, or weakness
These symptoms can come and go or remain constant, which makes it difficult for patients and doctors alike to pinpoint the root cause.
Potential causes
Autoimmune disorders are one cause of chronic systemic inflammation. In these conditions, the immune system mistakenly attacks healthy tissues, thinking they are threats. Examples include:
- Rheumatoid arthritis
- Vasculitis
- Inflammatory bowel disease (Crohn’s disease, ulcerative colitis)
Patients with rare diseases, such as Lupus, Multiple sclerosis and Eosinophilic Granulomatosis with Polyangiitis can also manifest this symptom.
Other triggers might be infections, metabolic conditions, and environmental factors. Because of this, identifying the underlying cause is crucial to guide proper treatment and improve patients’ lives.
Diagnosis
Diagnosis can be challenging because symptoms overlap with many other conditions. Doctors usually start with a detailed medical history and physical exam, followed by blood tests to check inflammatory markers (CRP, ESR) and immune cell counts.
If autoimmune causes are suspected, antibody tests such as ANCA may be used. Imaging like CT or MRI can identify inflammation in organs, and sometimes a tissue biopsy is needed to confirm. Tracking symptoms over time helps build the full picture.
Treatment Options
The treatment of chronic systemic inflammation depends on its underlying cause and the severity of symptoms. In cases involving autoimmune inflammation, the primary goal is to reduce immune system activity and prevent long-term damage to organs.
Treatment often begins with corticosteroids like prednisone to quickly bring down inflammation. For long-term management, immunosuppressive drugs such as methotrexate or azathioprine may be prescribed.
In more targeted approaches, biologic therapies like mepolizumab are used to block specific immune pathways involving eosinophils.
Alongside medication, lifestyle modifications can play an important role in managing chronic inflammation. Anti-inflammatory nutrition, regular physical activity, adequate sleep, and stress reduction strategies may help support immune regulation and improve daily well-being.
Because it can affect many organ systems, treatment often involves collaboration between various specialists, including rheumatologists, pulmonologists, neurologists, and primary care providers. Early and coordinated care can make a significant difference in outcomes and quality of life.
Take Action Now
If you’ve been experiencing these symptoms and suspect a rare diseases, we’re here to help you assess your risk.
Our expert medical team, supported by advanced AI-based tools, will carefully review your information and guide you toward the right care.
FAQ
What is chronic systemic inflammation?
It is a whole-body immune response that affects multiple organs and tissues. It occurs when the immune system stays activated over time, often without a clear trigger like infection or injury.
What does chronic inflammation feel like?
Chronic inflammation symptoms include fatigue, body pain, brain fog, skin issues, shortness of breath, and digestive problems. These symptoms can persist for weeks or months and are often subtle at first.
What diseases can cause chronic inflammation in the body?
Several conditions including autoimmune rare diseases (such as EGPA or Lupus), chronic infections, allergies, and metabolic disorders like obesity.